
HIPAA Consulting Services: Expert Answers & Guide
January 13, 2026|1:22 PM
Unlock Your Digital Potential
Whether it’s IT operations, cloud migration, or AI-driven innovation – let’s explore how we can support your success.

January 13, 2026|1:22 PM
Whether it’s IT operations, cloud migration, or AI-driven innovation – let’s explore how we can support your success.
Navigating healthcare regulations is tough for all kinds of organizations. It’s hard to keep patient info safe while keeping things running smoothly. This is where specialized help is needed.
With over $150 million in penalties and settlements, the risks are clear. Professional healthcare compliance consulting is key for avoiding big fines and keeping your reputation intact.
This guide is your go-to for HIPAA Consulting Services. It shows how expert advice makes complex rules work for your business. We aim to help you figure out what you need, understand your options, and set up strong privacy protection.
We’ll dive into how a solid HIPAA compliance program keeps your business safe. You’ll learn the benefits of working with seasoned consultants. And we’ll share practical steps to follow for lasting compliance.
In today’s healthcare world, creating a strong compliance program is key. It requires understanding the laws that protect protected health information everywhere. The rules of healthcare data compliance are complex. They demand that organizations know how to follow the rules while keeping their operations smooth.
We start by learning the basics of medical privacy regulations. This helps healthcare groups make smart choices about how to spend their resources on compliance.
The rules for protecting patient privacy have grown a lot since the 1990s. Knowing these rules helps organizations figure out what they need to do. They can then create plans that fit their specific situations.
The Health Insurance Portability and Accountability Act was passed in 1996. It set national standards for keeping patient health information safe. This law was made to help people keep their health insurance when they change jobs. It also made sure that patient data is protected everywhere in healthcare.
HIPAA applies to certain groups, like healthcare providers and health plans. It also covers companies that work with these groups, like billing companies and IT providers. These companies need to protect protected health information too.
At the heart of HIPAA is the idea of protected health information. This includes any health info that can identify a person. It’s not just names and social security numbers. It also includes things like IP addresses and photos linked to health records.
For a full HIPAA compliance guide, it’s important to understand how these ideas apply in everyday work. This helps in managing risks and following rules.
HIPAA has many rules that work together to protect patient privacy and data. The HIPAA Privacy Rule sets standards for who can see patient data and when it can be shared without permission.
The HIPAA Security Rule focuses on keeping electronic health information safe. It requires covered entities and their business partners to use strong measures to protect ePHI. This is because electronic data is more vulnerable than paper records.
There’s also a rule for reporting security breaches. It says that organizations must tell people whose data was lost, the government, and sometimes the media. The Enforcement Rule outlines how to investigate complaints and what penalties there are for not following the rules.
| HIPAA Component | Primary Focus | Key Requirements | Applies To |
|---|---|---|---|
| Privacy Rule | Use and disclosure of PHI | Patient rights, minimum necessary standard, authorization requirements | All forms of protected health information |
| Security Rule | Electronic data protection | Administrative, physical, and technical safeguards for ePHI | Electronic protected health information only |
| Breach Notification Rule | Incident reporting | Notification timelines, reporting thresholds, documentation standards | Unsecured PHI breaches |
| Enforcement Rule | Compliance oversight | Investigation procedures, penalty tiers, corrective action plans | All covered entities and business associates |
These rules work together to protect patient privacy. They cover both preventing problems and fixing them when they happen. Organizations need to have plans for each rule and make sure they all work together.
Following medical privacy regulations is very important. It’s not just about avoiding fines. It also builds trust with patients. When patients trust that their health information is safe, they are more likely to share it.
There are also financial reasons to follow the rules. Breaking them can cost a lot of money. For small practices, the fines can be devastating. For bigger places, it can still hurt a lot.
Staying compliant helps keep operations running smoothly. Investigations and penalties can disrupt work. They take staff away from caring for patients and may require big changes.
Being good at protecting data helps in the healthcare market. Patients, partners, and payers look at how well organizations protect data. Those that do well stand out and get more business.
Data breaches can hurt a company’s reputation for a long time. They can make it hard to keep patients, attract doctors, and get partnerships. Investing in healthcare data compliance helps keep a company’s reputation strong.
Professional HIPAA consulting services help bridge the gap between complex federal rules and practical application. They offer customized solutions that protect patient privacy and support growth. Healthcare entities face pressure to comply while keeping operations efficient. Our expertise turns complex rules into actionable strategies.
Our consulting partnership helps organizations tackle compliance challenges. This reduces risk and builds sustainable programs that adapt to changing rules.
Healthcare compliance consulting goes beyond simple checklists. It involves strategic planning, workforce development, and continuous improvement. Organizations get objective assessments to find vulnerabilities before they become violations. We provide the resources needed to close these gaps efficiently.
This approach ensures compliance aligns with clinical operations and business goals.
HIPAA consultants conduct thorough analyses to evaluate current practices against Privacy and Security Rule requirements. They identify areas needing improvement or remediation. Our gap assessments examine administrative, physical, and technical safeguards, providing detailed reports for prioritizing remediation.
Our teams develop customized policies and procedures that meet all regulatory mandates. These reflect each organization’s unique workflows and technology systems. We ensure documentation meets federal standards without burdening operations. We also establish protocols for handling protected health information.
Risk management strategies are a key focus. We implement systematic methods for identifying threats, evaluating vulnerabilities, and determining appropriate safeguards.
Workforce training is another critical service. We design and deliver education programs that prepare staff for their compliance responsibilities. Our training modules address practical scenarios employees face daily, ensuring security awareness is part of the culture. Training effectiveness directly correlates with compliance success, and we provide ongoing education to keep up with regulatory updates and emerging threats.
Managing business associates is a complex compliance requirement. We help organizations establish robust vendor oversight programs. We also develop incident response plans to prepare for potential breaches, ensuring timely detection and containment.
Our regulatory expertise includes breach notification requirements under federal and state laws.
| Consultant Function | Primary Activities | Organizational Impact | Compliance Outcome |
|---|---|---|---|
| Gap Analysis | Systematic evaluation of current practices against HIPAA requirements, vulnerability identification, risk scoring | Clear understanding of compliance status and remediation priorities | Reduced violation risk through proactive issue identification |
| Policy Development | Creating customized documentation for Privacy Rule and Security Rule compliance, procedure standardization | Consistent handling of protected information across all departments | Documented evidence of compliance efforts and organizational commitment |
| Risk Assessment | Threat identification, vulnerability evaluation, safeguard determination, risk mitigation planning | Strategic resource allocation based on actual risk exposure | Demonstrable risk management framework meeting Security Rule requirements |
| Training Programs | Role-based education development, awareness campaigns, competency verification, ongoing updates | Workforce preparedness and security culture establishment | Satisfied training documentation requirements and reduced human error incidents |
| Ongoing Monitoring | Compliance audits, effectiveness assessments, regulatory update integration, continuous improvement | Sustained adherence as operations and regulations evolve | Long-term compliance maintenance and audit readiness |
Engaging healthcare compliance consulting offers significant benefits. It brings specialized regulatory expertise that internal teams often lack. This focused knowledge accelerates compliance implementation and reduces the learning curve for organizations.
Cost-effectiveness is a key advantage. Hiring consultants eliminates the expense of maintaining full-time compliance staff. Organizations gain access to proven methodologies and best practices developed through experience across diverse healthcare settings.
Professional consultants manage compliance program implementation. They provide dedicated resources that keep initiatives on schedule and within budget. This focused approach prevents compliance projects from stalling due to competing priorities.
Leadership teams can concentrate on core healthcare delivery missions while we navigate regulatory complexities.
Risk reduction is perhaps the most compelling benefit. Consultants proactively identify and remediate compliance gaps before they result in breaches or financial penalties. This approach avoids the substantial costs associated with violations, including civil monetary penalties and reputational damage.
Our regulatory expertise transforms compliance into a strategic capability. It protects patient privacy, enhances operational efficiency, and supports sustainable business growth in the highly regulated healthcare industry.
Choosing the right HIPAA consulting firm is key to your organization’s success. It’s not just about finding the cheapest option. You need a firm that fits your needs and values. The best partner will help you stay compliant and improve your operations.
When choosing, look at many factors. Check their credentials and past work. Make sure they understand your specific challenges. A good partner will be an extension of your team, offering guidance and support.

Look for several key factors in a consulting firm. Compliance expertise is essential. Check if they have the right knowledge and experience.
First, check their credentials and certifications. Look for HIPAA certification and ongoing education. This shows they keep up with changes.
Next, see if they have experience with organizations like yours. This ensures they understand your specific challenges. Relevant experience is crucial.
Then, ask about their approach to compliance. They should offer customized solutions, not one-size-fits-all plans. This flexibility is important for your organization.
Consider these additional criteria:
Client references are very important. They can give you real insights into the firm’s work. Ask about their experience, challenges, and support.
Ask the right questions to assess a consultant’s expertise. Focus on their qualifications, approach, experience, and support.
Start with qualification verification: Ask about their credentials and how they stay updated. Inquire about their team’s education and certifications.
Then, ask about their experience. “What experience do you have with organizations like ours?” and “Can you provide client references?” These questions help you understand if they get your challenges.
Explore their methodology with questions like:
Clarify ongoing support expectations. Ask about their support after the initial work. Compliance is an ongoing process.
Address practical issues like pricing and what’s included. Clear financial arrangements are important for a smooth partnership.
By carefully evaluating and asking the right questions, you can find a partner that meets your needs. They will help you stay compliant and support your business goals.
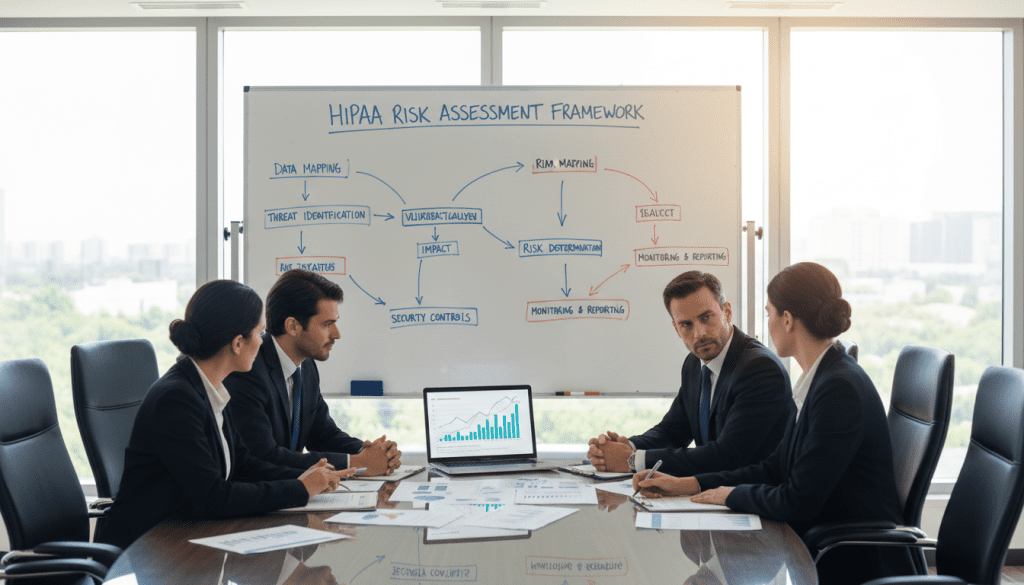
Healthcare organizations must keep up with regulatory rules to protect patient data. Regular HIPAA risk assessments are key to avoiding costly mistakes. These evaluations check your organization’s systems and security measures. HIPAA rules require covered entities to do and document risk assessments.
These assessments look at threats to patient data and find ways to protect it. We help find weaknesses before they cause big problems. This way, healthcare providers can fix issues quickly and save money.
Regular HIPAA risk assessments are very important today. Healthcare technology and rules change a lot. This means your organization’s security needs to keep up.
These evaluations help find and fix problems early. This saves a lot of money and trouble. Early detection is very valuable.
Regular checks help your organization stay safe. They show you’re serious about protecting patient data. They also help you focus on the most important security issues first. This makes sure your systems stay safe as they change.
Regular checks make your security better over time. This approach keeps your organization safe and up-to-date. It makes compliance a dynamic process that adapts to new challenges.
Experts use different ways to check if your organization is following the rules. No one method is enough. Using many methods gives a full picture of your compliance.
These checks look at all threats to patient data. They check your policies, physical security, and technology. They also find where you’re not following the rules.
They check your technology to find security weaknesses. They make sure your policies are up-to-date. They also check if your employees know how to follow the rules.
They look at how you work with third-party vendors. They test how ready you are for emergencies. This helps find problems before they happen.
| Assessment Method | Primary Focus Area | Key Deliverable | Recommended Frequency |
|---|---|---|---|
| Comprehensive Risk Analysis | All safeguard domains | Prioritized risk inventory | Annually |
| Compliance Gap Analysis | Regulatory requirements | Deficiency remediation plan | Bi-annually |
| Security Configuration Review | Technical safeguards | System hardening recommendations | Quarterly |
| Workforce Competency Evaluation | Employee knowledge | Training needs assessment | Annually |
Regular checks help your organization stay on top of compliance. This shows you’re serious about protecting patient data. It keeps you safe and in line with the rules.
Even the best security systems can’t replace well-trained staff. They need to know about privacy and HIPAA rules. This knowledge is key to protecting patient info every day.
Everyone who handles patient info must understand their role in keeping it safe. This includes receptionists, doctors, and billing staff. They need to know why following rules is important.
HIPAA says all staff must get trained on handling patient info. This includes employees, volunteers, and contractors. Training is a must to keep everyone on the same page.
Training records are kept for at least six years. This is to show proof of following rules during audits or investigations.
Seeing HIPAA training programs as just a formality is a big mistake. Good training turns rules into actions that staff can follow every day. We see training as a way to make our teams better, not just a rule to follow.
We design our training to make a lasting impact. It’s not just about knowing the rules. It’s about applying them in real-life situations.
Training isn’t just for new hires. It’s ongoing because rules and threats change all the time. Single training events cannot maintain workforce competency over time.
Training must keep up with new rules and threats. It should refresh basic privacy and security ideas. It should also teach about new policies and lessons from past mistakes.
Experts suggest a mix of training types. Annual big refreshers are good, but so are smaller sessions for specific issues. When roles change, staff need to know their new duties and how to keep info safe.
We make sure training is ongoing and varied:
We track all training activities. This includes who was trained, when, and what they learned. These records show we’re serious about following rules during audits or investigations.
Creating good training takes careful planning. It should engage and teach staff in ways that make sense for their jobs. Training that’s the same for everyone doesn’t work well.
We start with a deep look at what each job needs. This helps us focus on the right training for each role. This way, everyone knows their part in keeping info safe.
Our training is practical and clear. It explains the rules and why they matter. It uses real examples to make learning stick.
Choosing the right way to deliver training is key. It depends on the staff, technology, and how far apart they are. We pick methods that work best for everyone involved.
| Training Method | Best Applications | Key Advantages | Implementation Considerations |
|---|---|---|---|
| In-person instructor-led sessions | Complex topics requiring discussion and immediate clarification | Direct interaction, immediate questions, relationship building | Scheduling challenges, higher costs, geographic limitations |
| Online learning modules | Standardized content delivery across distributed workforce | Flexibility, consistency, automated tracking, cost efficiency | Requires technology access, less personal engagement |
| Blended approaches | Comprehensive programs combining multiple methods | Maximizes advantages of different formats, accommodates diverse learning styles | Increased complexity in design and administration |
| Microlearning and reinforcement | Ongoing awareness between formal training sessions | Regular touchpoints, bite-sized content, sustained engagement | Requires consistent content creation and distribution systems |
We tailor training to each role. Doctors learn about keeping patient info safe. IT staff get training on keeping systems secure. This way, everyone knows their part in keeping info safe.
Checking if staff really get it is important. We test their skills with real-life scenarios. If they don’t pass, they get more training.
We always look for ways to make training better. We ask staff for feedback and check if our training is working. This helps us keep training relevant and effective.
Investing in HIPAA training programs pays off in many ways. It reduces mistakes and keeps patient info safe. It also makes staff more committed to following rules. Training helps everyone work better together.
We work with organizations to make training a key part of their success. We help build a culture of security and empower staff to protect patient privacy every day.
We know that HIPAA compliance starts with a good risk analysis. It’s about protecting health data from new threats. A detailed HIPAA risk assessment is key to any good compliance program. It helps find weaknesses before they cause big problems.
Healthcare groups can then use cybersecurity safeguards to keep data safe. These steps make sure security and work flow go hand in hand.
This process turns big rules into real steps to keep data safe. Groups must always check their security to face new threats. This keeps health info safe and only shared with the right people.
We use detailed methods to find threats in all places where health info is stored. Looking at many types of threats helps find the biggest risks. Each threat needs a special plan to fix it.
Malicious external attacks are a big worry. Hackers want to get into health data. Groups must be ready for these attacks and have strong security.
Insider threats are also a big risk. Employees might share info they shouldn’t or make mistakes. We help groups watch for these issues without spying on their workers.
System failures can also be a problem. These failures can happen without warning and make data hard to get. Checking for these weaknesses helps avoid big problems.
Our method includes several steps:
Things like natural disasters can also be a problem. These events can destroy data or make systems fail. Groups need plans to keep data safe in these situations.
Weak policies or training can also be a problem. We check how groups teach their workers and enforce rules. This helps keep data safe.
We turn weaknesses into plans to fix them. Our method focuses on the biggest threats first. This way, groups can protect their data well without wasting resources.
Administrative safeguards set up the rules for security. Groups need to pick leaders for security and make clear rules. This keeps everyone on the same page.
Training helps workers know how to protect data. This training covers both how to do things right and why it’s important. We make training fun and keep it up to date.
Physical safeguards keep the place and equipment safe. Groups control who can get in and have rules for using devices. They also encrypt devices to keep data safe if they get lost.
Technical safeguards use technology to protect systems. Access controls check who’s getting in and limit what they can do. Logging all access helps catch problems.
Key tech protections include:
We help groups make sure they can get back to normal after a problem. This includes having backups and testing them. This way, groups can bounce back fast if something goes wrong.
Being ready to handle security problems is key. Groups need clear steps for finding and fixing problems. We help them get their teams ready and make plans for talking about problems.
Keeping an eye on things helps find new problems before they get big. We use tools to watch for trouble and alert groups right away. This makes HIPAA compliance a living thing that keeps up with new threats.
By really looking at risks and planning well, groups can keep patient info safe. This helps them avoid big problems and stay in line with rules. It makes sure groups can keep doing their work without worrying about security.
Starting with good HIPAA policies is key to following the rules. These policies make complex rules easy for your team to follow every day. They help protect patient info and set clear rules for your team.
These documents guide how your team works, show who is responsible, and show you care about keeping patient info safe. They are the backbone of your team’s actions.
Rules say you must keep these policies for at least six years. This shows you’re serious about following the rules when auditors come. We make sure your policies are real and work for your team, not just for the rules.
Good compliance documents cover all parts of your work. We make policies that fit your team’s real work, not just generic ones. This way, your team can follow them easily with what they already have.
Important documents include privacy rules, how to share patient info, and patient rights. They also name who is in charge of keeping things right and who to talk to if there’s a problem.
Security rules cover how to keep patient info safe from hackers. This includes training, how to handle problems, and keeping systems secure. It’s all about keeping patient info safe.
Your policies should also cover how to handle different situations. We suggest including these important parts:
The table below shows what documents you need to follow the rules and keep your team safe:
| Documentation Category | Key Components | Primary Purpose | Retention Period |
|---|---|---|---|
| Privacy Policies | Use and disclosure rules, patient rights, authorization procedures | Govern PHI handling and patient interactions | Minimum 6 years |
| Security Policies | Administrative, physical, and technical safeguards | Protect ePHI from unauthorized access | Minimum 6 years |
| Risk Assessments | Vulnerability identification, threat analysis, mitigation plans | Document security evaluation processes | Minimum 6 years |
| Incident Documentation | Breach reports, investigation findings, corrective actions | Track security events and responses | Minimum 6 years |
| Business Associate Agreements | Vendor contracts, security requirements, liability terms | Establish third-party compliance obligations | Duration of relationship plus 6 years |
Creating policies is not a one-time job. You need to keep them up to date. This ensures your team follows the right rules for your work and the changing rules.
Some things need you to check your policies. New rules or changes in how you work mean you need to update your policies. This keeps your team safe and following the rules.
New technology also means you need to update your policies. This includes new ways to store or share patient info. We suggest checking your policies when you get new tech to make sure it’s safe.
When you find problems, use them to make your policies better. If your team says something doesn’t work, listen and change it. Good policies are ones your team can follow, not just ones that look good on paper.
It’s also good to check your policies regularly. At least once a year, make sure they still work for your team. This helps you stay on top of new rules and best practices.
When you update your policies, do it right. Keep track of why you changed things and tell your team why. Make sure they understand the changes and that they agree to follow them.
By working on your policies, you make your team safer and more efficient. Your policies show you care about keeping patient info safe and that you’re serious about following the rules. This helps you avoid problems and shows you’re committed to protecting patient info.
In today’s digital healthcare world, picking the right technology is key. It helps protect patient info while keeping things running smoothly. Technology is the backbone for PHI security, helping healthcare groups meet rules and improve care.
Modern cybersecurity solutions must protect in many ways. They need to prevent, detect, and respond to threats. Choosing the right tech means looking at both short-term needs and long-term growth.
Healthcare leaders must show their tech protects patient data well. It’s not just about buying the right software. How it’s set up and managed is crucial for keeping data safe.
There are many tech solutions for healthcare compliance. We help find the right tools for each healthcare group. These tools must fit their needs and meet strict security standards.
Electronic health records compliance starts with the right EHR systems. These systems must have strong security features. They need to control who sees what, track all activity, and encrypt data.
Secure communication tools are also key. Digital messaging is used more in healthcare. Tools like HIPAA-compliant email and encrypted messaging apps keep messages safe.
Healthcare groups also need secure ways to share and store files. These tools protect documents and images with strong encryption. They help teams work together safely.
Telehealth platforms are important for virtual care. They must have secure video, document management, and identity checks. This ensures safe online consultations.
| Technology Category | Primary Functions | Key Security Features | Compliance Benefits |
|---|---|---|---|
| Electronic Health Records | Clinical documentation, care coordination, clinical decision support | Role-based access controls, audit logging, data encryption, automatic logoff | Centralized PHI security, comprehensive activity tracking, standardized workflows |
| Secure Communications | Provider messaging, patient engagement, care team collaboration | End-to-end encryption, message expiration, access authentication | Protected information exchange, documented communications, controlled distribution |
| Encryption Solutions | Data protection, device security, transmission safeguards | Full-disk encryption, file-level protection, network encryption protocols | Protection against unauthorized access, breach mitigation, regulatory requirement fulfillment |
| Access Management | Identity verification, permission controls, session management | Multi-factor authentication, single sign-on, automatic timeout, privilege management | Minimum necessary access, accountability mechanisms, reduced unauthorized access risk |
| Security Monitoring | Threat detection, incident response, compliance verification | Log aggregation, anomaly detection, real-time alerts, forensic analysis | Early breach detection, regulatory documentation, continuous improvement insights |
Practice management systems handle scheduling and billing. They also protect patient info. Security tools monitor systems for threats. Backup solutions keep data safe during system failures.
Choosing the right tech is just the start. Proper setup and management are key. Best practices cover the whole tech lifecycle.
Checking vendors is crucial. Look for security, compliance history, and Business Associate Agreements. Evaluate security certifications and audit reports.
Configuring systems right is important. Disable unnecessary features and use strong passwords. Set up audit logging to track activity.
Authentication mechanisms are vital. Use multi-factor authentication to add security. Make password policies strong but easy to remember.
Encryption technology must protect all electronic protected health information. Use full-disk encryption on devices and secure protocols for network communications.
Access controls should limit who sees what. Use role-based permissions and review access regularly. This keeps data safe and follows rules.
Mobile device management is key for smartphones and tablets. Enforce security policies, lock devices, and wipe data if lost. Restrict app installations to keep devices safe.
Remote access needs careful handling. Use virtual private networks and add extra authentication. Monitor remote connections for security issues.
Keeping software up to date is essential. Apply security patches quickly and test updates. Use current software versions to avoid security risks.
Regular security checks are important. They ensure PHI security is up to date. These checks help find and fix security issues.
The world of healthcare data compliance is changing fast. New technologies and stricter rules are putting pressure on organizations. The HHS Office for Civil Rights is now focusing more on small groups, leading to higher fines.
Over $150 million in fines show the cost of not following HIPAA rules. With inflation, these fines will only get higher. This means organizations must protect data more than ever.
Modern tech like connected medical devices and IoT expands attack areas. Common mistakes include unsecured emails and lost devices. Cyberattacks on healthcare are getting smarter, making constant security updates crucial.
AI in healthcare raises privacy concerns. It challenges old consent rules, needing new approaches to keep patient data safe. This balance is key for innovation and privacy.
We guide organizations to innovate in compliance with zero-trust security. This method checks all access requests. Advanced systems detect threats early, and tools monitor systems in real-time.
Privacy-by-design makes data protection a part of tech development. HIPAA compliance is now seen as a way to grow and protect patient trust. It’s not just a rule, but a competitive edge.
HIPAA is a law from 1996 that protects patient health information. It sets standards for sharing and keeping this information safe. HIPAA helps healthcare organizations build trust with patients and avoid big fines.
It also helps protect the organization’s reputation and keeps operations running smoothly. HIPAA is important for staying competitive in the digital healthcare world.
HIPAA consultants do many important things. They help identify and fix compliance gaps. They also create policies and procedures that follow HIPAA rules.
They conduct risk assessments and train the workforce. They also help manage business associates and create plans for handling breaches. This helps organizations stay compliant without having to hire full-time experts.
The cost of HIPAA consulting varies. It depends on the organization’s size, complexity, and the services needed. It’s important to look at the value and risk mitigation.
Consulting can be done on a project basis, hourly, or through retainer agreements. While it’s an investment, it’s worth it to avoid fines and maintain compliance.
The time it takes to become HIPAA compliant varies. It depends on the organization’s current status, size, and technology. It also depends on the scope of changes needed.
Small organizations might need three to six months. Larger ones might take longer. Compliance is an ongoing process that requires continuous monitoring and updates.
Look for certifications like CHPS, CHC, CISSP, and CIPP. These show the consultant’s knowledge and experience. It’s also important to check their experience working with similar organizations.
Check their track record and methodology. A good consultant will understand your organization’s needs and balance compliance with operational efficiency.
The frequency of risk assessments depends on several factors. It’s important to balance regulatory requirements with practical considerations. Annual assessments are a good starting point.
Additional assessments are needed for significant changes or security incidents. Ongoing monitoring is also important to stay aware of vulnerabilities.
Common violations include inadequate risk analyses and insufficient access controls. They also include lack of encryption and poor business associate agreements.
Professional consultants can help by conducting thorough risk assessments and implementing strong safeguards. They also provide training and ongoing monitoring to prevent breaches.
Small healthcare practices need HIPAA consulting services just as much as large ones. They face unique challenges due to limited resources and expertise.
Consultants provide specialized knowledge and help with compliance. They also help with risk assessments and training. This ensures small practices can focus on patient care while staying compliant.
If a breach is discovered, immediate action is needed. This includes containing the incident and assessing its impact. It’s also important to notify affected individuals and the Department of Health and Human Services.
Professional consultants can help with the investigation and notification process. They also assist with developing a plan to prevent future breaches.
Business associate agreements (BAAs) are crucial for HIPAA compliance. They ensure that vendors and partners protect patient information. Consultants can help with creating BAAs and managing vendor relationships.
They also conduct risk assessments and provide training. This helps organizations maintain compliance and protect patient information.
HIPAA violations can result in significant fines. The amount depends on the severity of the violation and the organization’s response. Penalties range from 0 to ,000 per violation, with a maximum of
HIPAA is a law from 1996 that protects patient health information. It sets standards for sharing and keeping this information safe. HIPAA helps healthcare organizations build trust with patients and avoid big fines.
It also helps protect the organization’s reputation and keeps operations running smoothly. HIPAA is important for staying competitive in the digital healthcare world.
HIPAA consultants do many important things. They help identify and fix compliance gaps. They also create policies and procedures that follow HIPAA rules.
They conduct risk assessments and train the workforce. They also help manage business associates and create plans for handling breaches. This helps organizations stay compliant without having to hire full-time experts.
The cost of HIPAA consulting varies. It depends on the organization’s size, complexity, and the services needed. It’s important to look at the value and risk mitigation.
Consulting can be done on a project basis, hourly, or through retainer agreements. While it’s an investment, it’s worth it to avoid fines and maintain compliance.
The time it takes to become HIPAA compliant varies. It depends on the organization’s current status, size, and technology. It also depends on the scope of changes needed.
Small organizations might need three to six months. Larger ones might take longer. Compliance is an ongoing process that requires continuous monitoring and updates.
Look for certifications like CHPS, CHC, CISSP, and CIPP. These show the consultant’s knowledge and experience. It’s also important to check their experience working with similar organizations.
Check their track record and methodology. A good consultant will understand your organization’s needs and balance compliance with operational efficiency.
The frequency of risk assessments depends on several factors. It’s important to balance regulatory requirements with practical considerations. Annual assessments are a good starting point.
Additional assessments are needed for significant changes or security incidents. Ongoing monitoring is also important to stay aware of vulnerabilities.
Common violations include inadequate risk analyses and insufficient access controls. They also include lack of encryption and poor business associate agreements.
Professional consultants can help by conducting thorough risk assessments and implementing strong safeguards. They also provide training and ongoing monitoring to prevent breaches.
Small healthcare practices need HIPAA consulting services just as much as large ones. They face unique challenges due to limited resources and expertise.
Consultants provide specialized knowledge and help with compliance. They also help with risk assessments and training. This ensures small practices can focus on patient care while staying compliant.
If a breach is discovered, immediate action is needed. This includes containing the incident and assessing its impact. It’s also important to notify affected individuals and the Department of Health and Human Services.
Professional consultants can help with the investigation and notification process. They also assist with developing a plan to prevent future breaches.
Business associate agreements (BAAs) are crucial for HIPAA compliance. They ensure that vendors and partners protect patient information. Consultants can help with creating BAAs and managing vendor relationships.
They also conduct risk assessments and provide training. This helps organizations maintain compliance and protect patient information.
HIPAA violations can result in significant fines. The amount depends on the severity of the violation and the organization’s response. Penalties range from $100 to $50,000 per violation, with a maximum of $1.5 million per violation category.
Professional consultants help organizations avoid these penalties. They develop compliance programs and conduct risk assessments. This ensures that organizations can focus on patient care without worrying about fines.
HIPAA has different rules for electronic and paper records. The Privacy Rule applies to all formats, ensuring consistent protection. The Security Rule focuses on electronic records, requiring specific safeguards.
Professional consultants help organizations implement these rules. They develop policies and conduct risk assessments. This ensures that both electronic and paper records are protected.
Cloud services can be used in healthcare, but careful selection is necessary. Organizations must ensure that vendors meet HIPAA requirements. This includes executing business associate agreements and implementing appropriate safeguards.
Professional consultants help with this process. They assess vendor capabilities and develop cloud-specific policies. This ensures that patient information is protected in the cloud.
New technologies like AI, IoT, and blockchain create compliance challenges. They require careful risk assessments and implementation of appropriate safeguards. Professional consultants help navigate these challenges.
They develop governance frameworks and implement privacy-by-design principles. This ensures that patient information is protected in complex technological environments.
Balancing compliance with operational efficiency is possible. It requires strategic approaches and engagement with clinical staff. Professional consultants help design compliance programs that respect operational realities.
They also help streamline workflows and implement user-friendly technologies. This ensures that compliance does not hinder patient care or operational efficiency.
.5 million per violation category.
Professional consultants help organizations avoid these penalties. They develop compliance programs and conduct risk assessments. This ensures that organizations can focus on patient care without worrying about fines.
HIPAA has different rules for electronic and paper records. The Privacy Rule applies to all formats, ensuring consistent protection. The Security Rule focuses on electronic records, requiring specific safeguards.
Professional consultants help organizations implement these rules. They develop policies and conduct risk assessments. This ensures that both electronic and paper records are protected.
Cloud services can be used in healthcare, but careful selection is necessary. Organizations must ensure that vendors meet HIPAA requirements. This includes executing business associate agreements and implementing appropriate safeguards.
Professional consultants help with this process. They assess vendor capabilities and develop cloud-specific policies. This ensures that patient information is protected in the cloud.
New technologies like AI, IoT, and blockchain create compliance challenges. They require careful risk assessments and implementation of appropriate safeguards. Professional consultants help navigate these challenges.
They develop governance frameworks and implement privacy-by-design principles. This ensures that patient information is protected in complex technological environments.
Balancing compliance with operational efficiency is possible. It requires strategic approaches and engagement with clinical staff. Professional consultants help design compliance programs that respect operational realities.
They also help streamline workflows and implement user-friendly technologies. This ensures that compliance does not hinder patient care or operational efficiency.
Experience power, efficiency, and rapid scaling with Cloud Platforms!